Chimeric antigen receptor (CAR) T-cell therapy is a groundbreaking form of immunotherapy that has revolutionized cancer treatment. By harnessing the power of a patient’s own immune system, CAR-T therapy offers hope to individuals battling various types of cancer. In this article, we delve into the science behind CAR-T cell therapy, its mechanism of action, and its impact on cancer patients.
What Is CAR-T Cell Therapy?
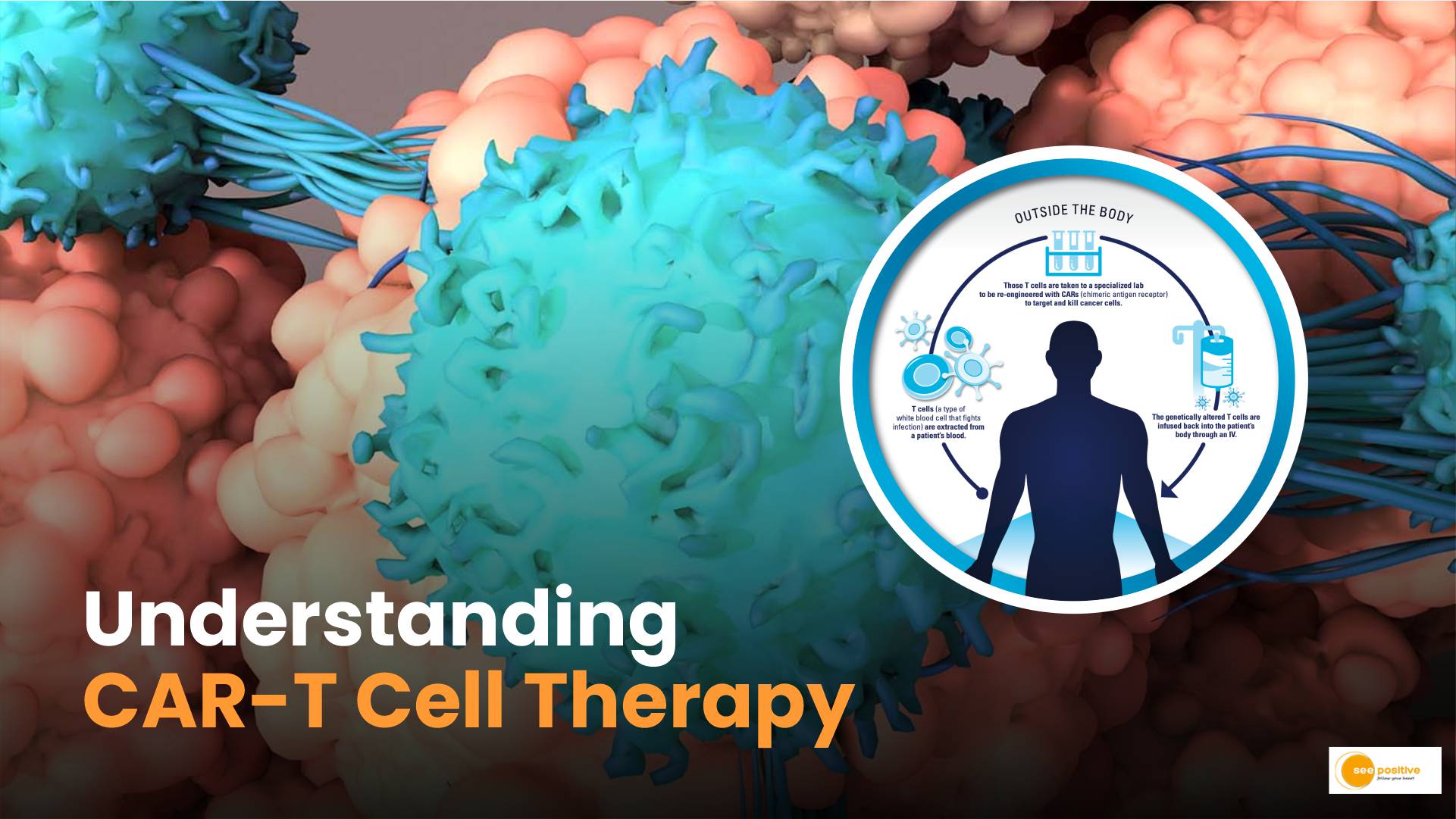
CAR-T cell therapy involves modifying a patient’s immune cells (specifically T cells) to enhance their ability to recognize and destroy cancer cells. Let’s break down the process step by step:
- T Cell Collection: First, T cells are extracted from the patient’s blood. These T cells play a crucial role in the immune response, defending the body against infections and abnormal cells.
- Genetic Modification: In the laboratory, scientists introduce a gene that encodes a chimeric antigen receptor (CAR) into the T cells. The CAR is a synthetic protein designed to recognize specific cancer cell antigens.
- CAR Structure: The CAR consists of three essential components:
- Antigen Recognition Domain: This part of the CAR recognizes and binds to cancer cell antigens.
- Intracellular Signaling Domains: These domains activate the T cell when the CAR binds to its target antigen.
- Transmembrane Domain: Anchors the CAR to the T cell membrane.
- Creating CAR T Cells: Once the T cells express the CAR, they become CAR T cells. These modified cells are now equipped to seek out cancer cells.
How Do CAR T Cells Work?
- Targeting Cancer Cells: CAR T cells circulate throughout the body, scanning for cancer cells. When they encounter a cancer cell displaying the specific antigen recognized by the CAR, they bind to it.
- Activation and Proliferation: Upon binding to the cancer cell, the CAR T cell becomes activated. It multiplies rapidly, creating a population of CAR T cells.
- Cytokine Release: Activated CAR T cells release signaling proteins called cytokines. These cytokines attract other immune cells to the site of the cancer cell.
- Inflammatory Response: The combined action of cytokines and activated T cells leads to significant inflammation focused on the cancer cell. This inflammatory response causes the cancer cell to undergo apoptosis (cell death).
- Remission: If CAR T cells successfully eliminate all cancer cells, the patient achieves remission, meaning the cancer disappears either temporarily or permanently.
Which types of cancer is CAR T-cell therapy approved for?
Even though approvals around CAR T-cell therapy are rapidly changing, the types of cancer that are currently treated using this method include:
- Diffuse large B-cell lymphoma
- Follicular lymphoma
- Mantle cell lymphoma
- Multiple myeloma
- B-cell acute lymphoblastic leukemia
Patient Experience with CAR-T Cell Therapy
- Referral to Specialized Centers: Patients with cancer must be referred to specialized centers offering CAR-T cell therapy.
- T Cell Collection: The patient’s T cells are collected, often after previous cancer treatment. These T cells may not be as healthy due to prior therapies.
- Laboratory Modification: In the lab, the T cells receive the CAR modification.
- Infusion: After a few weeks, the patient receives an infusion of the modified CAR T cells. These cells then recognize and attack cancer cells.
Conclusion
CAR-T cell therapy represents a remarkable advancement in cancer treatment. By reprogramming the patient’s immune system, it offers hope to those who previously had limited options. As research continues, CAR-T therapy holds promise for even more cancer types and improved outcomes.
Remember, each patient’s journey is unique, and ongoing research aims to refine and expand the application of CAR-T cell therapy. With this groundbreaking approach, we move closer to a future where cancer becomes a manageable disease rather than a life-threatening one.